Understanding sperm DNA fragmentation testing: Methods, reliability, and clinical relevance
When it comes to assessing male fertility, most people are familiar with a semen analysis looking at sperm count, motility, and morphology. But these measures don't tell the whole story and are not predictive of the male fertility potential as the standard semen analysis, even according to WHO criteria, is subjective and susceptible to numerous errors (Esteves,2014; Wang & Swerdloff, 2014; Douglas et al., 2021; Sanyal et al., 2023). Therefore, clinicians and scientists are increasingly looking at other parameters including sperm DNA fragmentation, a critical factor that can affect fertility even when semen parameters appear normal (Repalle et al., 2022; Sugihara etal., 2022; Wang et al., 2023; Stavros et al., 2024).
DNA fragmentation tests evaluate the integrity of genetic material in sperm, a key component for successful fertilisation, healthy embryo development, and even live birth outcomes. In this article, we’ll explore the most widely used DNA fragmentation tests, discuss their differences, and help patients understand when and why one might be chosen over another.
What is sperm DNA fragmentation?
DNA fragmentation refers to the presence of breaks or irregularities in the genetic material within a sperm cell. This damage can occur during sperm production (spermatogenesis), whilst sperm are stored in the epididymis or during the process of ejaculation.
The damage can result from:
- Oxidative stress
- Environmental toxins
- Heat exposure
- Infections
- Varicoceles
- Ageing
- Lifestyle factors (e.g., smoking, poor diet, hot baths, excessive cycling)
- Radiation (X-rays, cell phones in the pocket etc.)
High levels of fragmentation are associated with:
- Poor embryo quality
- Implantation failure
- Miscarriage
- Lower success rates in IVF/ICSI cycles
That’s why understanding and accurately measuring DNA fragmentation has become a vital tool in diagnosing and managing male infertility.
When should you consider a DNA fragmentation test?
Sperm DNA fragmentation testing isn’t always the first step in fertility assessments but in certain situations, it can offer vital insights that a standard semen analysis can’t.
If you're facing ongoing challenges in your fertility journey, this type of testing may help uncover hidden issues that affect embryo development, implantation, or pregnancy success.
You may want to consider a sperm DNA fragmentation test if:
- You’ve had multiple IVF or ICSI failures
Even if fertilisation has occurred, embryos may fail to implant or develop due to compromised sperm DNA integrity. A fragmentation test can help identify if this is a factor. - You’ve experienced recurrent miscarriage
Repeated pregnancy loss especially when other causes have been ruled out can sometimes be linked to damaged sperm DNA contributing to embryo failure. - You’ve been told you have unexplained infertility
If standard fertility tests come back normal, but pregnancy still isn’t happening, a fragmentation test can uncover issues that would otherwise go undetected. - You’re over the age of 40
As men age, the likelihood of sperm DNA damage increases, even if other semen parameters remain within normal ranges. - You have lifestyle or environmental risk factors
Smoking, high alcohol intake, obesity, chronic stress, poor diet, pollution, or frequent heat exposure (like hot baths or laptops on the lap) can all increase DNA damage. - You have a varicocele
Varicoceles, enlarged veins in the scrotum, can lead to elevated scrotal temperatures and oxidative stress, both of which are linked to DNA fragmentation. - You’ve had previous infections or medical treatments
Infections in the reproductive tract, fevers, or exposure to certain medications (including chemotherapy) can all increase DNA damage in sperm. - You’ve undergone testicularsurgery or trauma
Physical injury or surgical history affecting the testicles can compromise sperm DNA integrity.
In these situations, DNA fragmentation testing could help clarify next steps, guide treatment planning, or highlight opportunities to improve sperm quality before pursuing fertility treatment (Çağlayan et al., 2022;Repalle et al., 2022; Sugihara et al., 2022; Wang et al., 2023; Stavros et al.,2024).
Why lab quality is non-negotiable
Before diving into the tests themselves, it's essential to understand why laboratory quality and accreditation matter. Sperm DNA fragmentation testing is highly complex and sensitive, and results can vary dramatically between labs.
Testing requires:
- Validated methods
- Accredited laboratories
- Trained andrology professionals
Without these standards, patients risk getting misleading results that may delay or misdirect fertility treatment. Always ensure the testis done in a validated, clinically accredited laboratory with transparent quality control procedures otherwise you may end up finding yourself having to repeat the test elsewhere.
How do sperm DNA fragmentation tests work?
Let’s explore the main clinically used tests, how they work, their pros and cons, and when they’re appropriate (Agarwal et al., 2024).
1. SCSA (Sperm Chromatin Structure Assay)
How it works:
For the SCSA, the sperm DNA is denatured by an acid. The DNA is then stained with a dye (acridine orange), which fluoresces differently depending on whether the DNA is intact (green fluorescence) or fragmented (orange-red fluorescence).The analysis is done using flow cytometry to assess the susceptibility of sperm DNA to acid-induced denaturation. This has the advantage that a large number of sperm (usually 5,000 to 10,000) can be analysed in a relatively short period of time. The system is automated and is therefore eliminating subjectivity. The test measures both single- and double-strand DNA breaks. The result is a DNA Fragmentation Index (DFI; the percentage of sperm with fragmented or damaged DNA), a reliable measure of the percentage of sperm with fragmented DNA.
Strengths:
- Highly standardised and reproducible
- High repeatability
- Evaluated in a number of different studies
- Can analyse thousands of sperm rapidly
- Offers clear, quantitative results
- Available and affordable in the UK
- Strong clinical validation confirmed in a meta-analysis
- Fresh and frozen samples can be analysed
- Second-most frequently requested test by practitioners, globally
Weaknesses:
- Requires specialist equipment and trained staff
- Measures potential DNA damage
When to use:
Ideal for patients undergoing ART (especially ICSI), recurrent miscarriage cases, and unexplained infertility. Particularly useful when needing a quantitative, research-backed test.
2. TUNEL – Terminal deoxynucleotidyl transferase dUTP nick end labelling
How it works:
TUNEL labels broken DNA strands directly with fluorescent markers and is visualised using light microscopy, fluorescence microscopy or with flowcytometry. When microscopic techniques are employed, only a relatively small number of sperm (usually 200 to 500) is evaluated, whereas using flowcytometry 5,000 to 10,000 sperm are analysed. Like the SCSA, the TUNEL assay measures both single- and double-strand DNA breaks. The result is expressed percentage of sperm with fragmented or damaged DNA.
Strengths:
- Measures real DNA damage
- Used widely in research and advanced clinics
- Sensitive and reliable
- Evaluated in a number of different studies
- Analysis of thousands of sperm rapidly
- Minimal inter-observer variability
- Offers clear, quantitative results
- Available and affordable in the UK
- Strong clinical validation confirmed in a meta-analysis
- Fresh and frozen samples can be analysed
- Most frequently requested by practitioners, globally
Weaknesses:
- Technically more challenging than the SCSA
- Results vary between techniques (microscopy vs. flow cytometry)
- Less standardised than SCSA
- Different protocols to perform the test are available
When to use:
Well-suited to research settings, complex clinical cases, or where detailed quantification is required. In addition, the test is useful for patients undergoing ART with recurrent miscarriage and unexplained infertility. Particularly useful when needing a quantitative, research-backed test.
3. COMET Test – Single Cell Gel Electrophoresis (Examen)
How it works:
Sperm are suspended in an agarose gel, spread on a microscopic slide and exposed to an electric field. If the DNA is damaged, the small DNA fragments move out of the nucleus and form a "comet tail" visible under a microscope. The longer the tail, the more damage. Depending on which type of the COMET assay, neutral or alkaline, is used, the test measures real and potential DNA damage, respectively. The COMET assay measures total DNA fragmentation and is also able to distinguish between single- and double-strand breaks of the DNA. While single-strand breaks can be repaired by the oocyte, this is harder, if not impossible, for double-strand breaks.
Strengths:
- Discrimination between single-and double-strand breaks is possible
- Correlation with semen parameters
- Highly sensitive and detailed
Weaknesses:
- Labour-intensive and not yet standardised
- Poorly repeatable
- High inter-observer and inter-laboratory variability
- Time-consuming
- Only a relatively small number of sperm is analysed
- Requires expert lab handling
- High costs
When to use:
Best in specialised research settings or for detailed analysis when greater detail for the type of DNA damage is needed, especially in complex cases or for the need to identify double-strand breaks specifically.
4. SCD – Sperm Chromatin Dispersion Test (branded version HALO)
How it works:
Like for the SCSA, this test uses a chemical process to denature sperm DNA. The sample is then suspended in an agarose gel on a microscopic slide and incubated. If the DNA is intact, a "halo" forms around the sperm nucleus. Damaged DNA prevents halo formation, indicating fragmentation. A relatively small number of sperm (usually 200 to 500) is microscopically evaluated.
Strengths:
- Simple and cost-effective
- Quick and accessible
- Repeatable with consistent results
- Evaluated in a number of different studies
- Commercial kit available
- Frequently requested by practitioners, globally
Weaknesses:
- Highly subjective and operator-dependent
- Inter-observer and inter-laboratory variability
- Low clinical reliability
- Not recommended for major fertility decisions
When to use:
May be used for basic screening in low-resource settings but should not be relied upon for major clinical decision-making.
Choosing the right test
With multiple testing options available, it’s natural to feel unsure about which test is most suitable. The truth is, there’s no one-size-fits-all answer. The right test depends on your medical history, fertility journey, and what you (and your clinician) need the test to tell you.
Here are a few important things to consider:
- What’s your fertility history?
If you’ve experienced failed IVF/ICSI cycles or recurrent miscarriage, a more detailed and clinically validated test may be necessary. - What information are you looking for?
Are you simply screening for damage or do you need to understand the type and extent of DNA damage? Some tests give broader clinical insights than others. - Will yourresults be used to guide clinical treatment?
If your results will influence decisions about IVF, ICSI, or surgery, it's vital to choose a well-validated and widely accepted test.
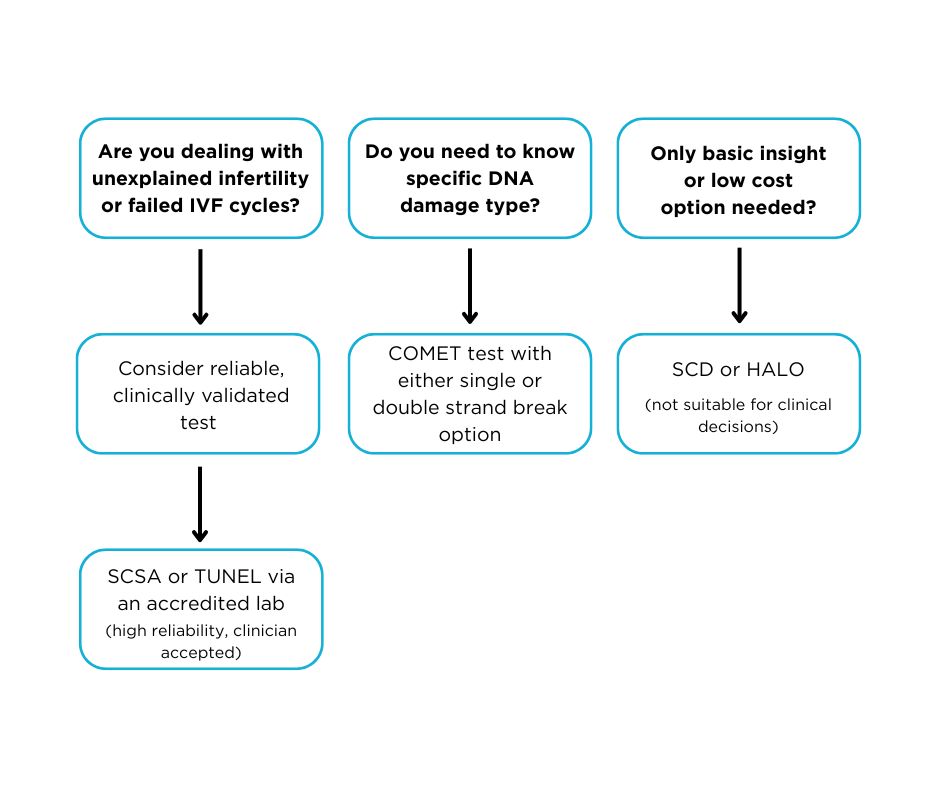
To help you navigate this, here’s a simple flow chart outlining when each type of test may be most appropriate:
What should you do after receiving your DNA fragmentation results?
Getting the results of a sperm DNA fragmentation test can be both illuminating and overwhelming. Whether your result shows high, moderate, or low fragmentation, what you do next matters more than the number itself.
High DNA fragmentation doesn't mean you're infertile, but itis a sign that something is interfering with sperm quality. It’s not necessarily a permanent state but the correct investigations and treatment are important.
Your next move should be a consultation with a male fertility specialist (an andrologist or urologist). They can help:
- Interpret your result in the context of your overall fertility profile
- Identify and treat possible underlying causes
- Guide you through diagnostic follow-ups
Many couples are told by the fertility clinic that ICSI (Intracytoplasmic Sperm Injection) is the solution to DNA fragmentation. Since ICSI doesn’t repair DNA and only bypasses the oocyte vestments, it is NOT a solution. Yes, it is correct that the probability of fertilisation can be increased by ICSI as specific sperm separation techniques that are able to enrich good quality sperm for the injection. However, this procedure does not solve the problem of highly DNA-fragmented sperm being produced. Therefore, the route course of the DNA damage should be diagnosed and treated first.
If the sperm’s DNA is damaged, ICSI may still result in:
- Poor embryo quality
- Failed implantation
- Miscarriage
That’s why it's critical to address the underlying causes first, wherever possible, before turning to an invasive and more costly fertility treatment.
There are many ways men can actively improve DNA integrity. Depending on the cause, your fertility specialist may suggest:
- Lifestyle changes
- Antioxidant therapy
- Surgical correction of issues like varicocele
- Avoidance of toxins and heat
- Hormonal balancing
- Shorter abstinence periods
After 3–6 months (and in some cases longer) of targeted intervention, you may be advised to repeat the DNA fragmentation test. Sperm quality can change with time, lifestyle adjustments, and even the season. So, it’s important to measure progress objectively.
Once you’ve taken steps to improve your sperm quality and retested, your male fertility specialist will advise on further steps, this maybe to continue to try naturally or to move to IVF with or without ICSI.
At this point, if fertility treatment is still needed, you can enter it with greater confidence that you’ve optimised your sperm health which may improve success rates, reduce costs, and protect your emotional wellbeing.
DNA fragmentation isn’t the end of the road, it’s a signpost. With the right investigation, guidance, and support, many men are able to improve their sperm DNA and naturally or successfully conceive with less invasive treatment.
Conclusion
Sperm DNA fragmentation testing has transformed the way we assess male fertility. But not all tests are created equal. While SCSA and TUNEL offer greater clinical accuracy, tests like the SCD may lack the robustness needed for reliable diagnosis.
Just as important as the test itself is where and how it’s carried out. Lab accreditation, validation, and procedural consistency are essential to ensure the results are meaningful and accepted by clinicians.
Lastly, no test result should be viewed in isolation. The right test, performed in the right setting, and supported by professional guidance, can provide clarity and direction in the often-complicated world of fertility.
References
- Agarwal A, Farkouh A, Saleh R, Hamoda TAAAM, Salvio G,Boitrelle F, Harraz AM, Ghayda RA, Kavoussi P, Gül M, Toprak T, Russo GI,Durairajanayagam D, Rambhatla A, Birowo P, Cannarella R, Phuoc NHV, Zini A,Arafa M, Wyns C, Tremellen K, Sarıkaya S, Lewis S, Evenson DP, Ko E, CalogeroAE, Bahar F, Martínez M, Ambar RF, Colpi GM, Bakircioglu ME, Henkel R, KandilH, Serefoglu EC, Alfakhri A, Tsujimura A, Kheradmand A, Marino A, Adamyan A,Zilaitiene B, Ozer C, Pescatori E, Vogiatzi P, Busetto GM, Balercia G, ElbardisiH, Akhavizadegan H, Sajadi H, Taniguchi H, Park HJ, Maldonado Rosas I,Al-Marhoon M, Gilani MAS, Alhathal N, Quang N, Pinggera GM, Kothari P, Micic S,Homa S, Long TQT, Zohdy W, Atmoko W, Ibrahim W, Sabbaghian M, Abumelha SM,Chung E, Ugur MR, Ozkent MS, Selim O, Darbandi M, Fukuhara S, Jamali M, de laRosette J, Kuroda S, Smith RP, Baser A, Kalkanli A, Tadros NN, Aydos K, MierzwaTC, Khalafalla K, Malhotra V, Moussa M, Finocchi F, Rachman RI, Giulioni C,Avidor-Reiss T, Kahraman O, Çeker G, Zenoaga-Barbăroşie C, Barrett TL, YilmazM, Kadioglu A, Jindal S, Omran H, Bocu K, Karthikeyan VS, Franco G, SolorzanoJF, Vishwakarma RB, Arianto E, Garrido N, Jain D, Gherabi N, Sokolakis I,Palani A, Calik G, Kulaksiz D, Simanaviciene V, Simopoulou M, Güngör ND,Blecher G, Falcone M, Jezek D, Preto M, Amar E, Le TV, Ahn ST, Rezano A, SinghA, Rocco L, Savira M, Rajmil O, Darbandi S, Sogutdelen E, Boeri L, Hernández G,Hakim L, Morimoto Y, Japari A, Sofikitis N, Altay B, Mahmutoglu AM, Al HashimiM, Ziouziou I, Anagnostopoulou C, Lin H, Shah R (2024); Technical aspects andclinical limitations of sperm DNA fragmentation testing in male infertility: Aglobal survey, current guidelines, and expert recommendations. World J MensHealth 42: 202-215
- Douglas C, Parekh N, Kahn LG, Henkel R, Agarwal A (2021); Anovel approach to improving the reliability of manual semen analysis: Aparadigm shift in the workup of infertile men. World J Mens Health 39: 172-185
- Esteves SC (2014); Clinical relevance of routine semenanalysis and controversies surrounding the 2010 World Health Organizationcriteria for semen examination. Int Braz J Urol 40: 443-453
- Repalle D, Saritha KV, Bhandari S (2022); Sperm DNAfragmentation negatively influences the cumulative live birth rate in theintracytoplasmic sperm injection cycles of couples with unexplainedinfertility. Clin Exp Reprod Med 49(3): 185-195
- Sanyal D, Arya D, Nishi K, Balasinor N, Singh D (2023);Clinical utility of sperm function tests in predicting male fertility: Asystematic review. Reprod Sci 31: 863-882
- Stavros S, Potiris A, Molopodi E, Mavrogianni D, ZikopoulosZ, Louis K, Karampitsakos T, Nazou E, Sioutis D, Christodoulaki C, Skentou C,Gerede A, Zachariou A, Christopoulos P, Panagopoulos P, Domali E, Drakakis P(2024); Sperm DNA fragmentation: Unraveling its imperative impact on maleinfertility based on recent evidence. Int J Mol Sci 25(18): 10167
- Sugihara A, Punjabi U, Roelant E, De Neubourg D (2022); Isthere a relationship between sperm DNA fragmentation and intra-uterineinsemination outcome in couples with unexplained or mild male infertility?Results from the ID-Trial. Life (Basel) 13(1): 11
- Wang C, Swerdloff RS (2014); Limitations of semen analysisas a test of male fertility and anticipated needs from newer tests. FertilSteril 102: 1502-1507
- Wang Q, Gu X, Chen Y, Yu M, Peng L, Zhong S, Wang X, Lv J(2023); The effect of sperm DNA fragmentation on in vitro fertilizationoutcomes of unexplained infertility. Clinics (Sao Paulo) 78: 100261














.png)


